FREE SHIPPING OVER $50
Warning for Women Over 50: The 1 Common Supplement That Accelerates Bone Loss, Says Geriatrician

If you are a woman over 50, your focus on health naturally shifts toward preserving bone density. You probably take your vitamins seriously, buying the recommended supplements to protect yourself against osteoporosis, the silent condition that makes bones fragile and increases the risk of serious fractures. We are constantly bombarded with messages promoting various pills and powders, but what if one of the most common supplements you might be taking is actually doing more harm than good?
According to leading Geriatricians and bone health specialists, there is one popular mineral supplement—often taken with the best intentions—that can actually accelerate bone loss and interfere with the essential nutrients needed for true longevity. This is a crucial warning because, at this age, every step you take in your wellness journey needs to be strategic. It’s time to stop wasting your money and potentially damaging your skeletal health. Let’s uncover the identity of this surprising culprit and learn how to secure your bone future.
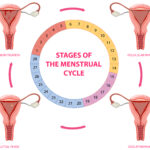
The Menopause Effect: Why Bone Health is Critical After 50
To understand the severity of this warning, we must first recognize the physiological reality for women over 50. The transition through menopause causes a sharp decline in estrogen. Estrogen plays a vital role in maintaining the balance between bone breakdown (resorption) and bone building (formation). When estrogen levels drop, the rate of bone breakdown dramatically outpaces formation, leading to accelerated bone loss.
This period of rapid loss makes the nutritional environment of your body incredibly sensitive. Any supplements or vitamins you introduce must work synergistically to support the remaining bone structure. Geriatricians emphasize that introducing a large dose of the wrong mineral can throw off the delicate balance with other crucial nutrients like magnesium and vitamin K2, ultimately making the problem of accelerating bone loss worse, not better.
The Supplement Culprit: High-Dose Elemental Calcium
The 1 common supplement that Geriatricians urge women over 50 to approach with extreme caution is high-dose elemental calcium—often taken alone or in excess of the necessary daily intake.
For years, doctors advised older women to take very large doses of calcium pills. However, modern research has painted a much more nuanced, and frankly alarming, picture. The problem isn’t calcium itself—it’s essential for bones—but the way we supplement it and the massive amounts often recommended.
How High-Dose Calcium Accelerates Bone Loss
Taking excessive amounts of supplemental calcium can actually backfire on bone health due to its interaction with other critical minerals and vitamins.
- Magnesium Displacement: Calcium and Magnesium compete for absorption in the gut. When you flood your system with high-dose calcium, it can hinder the absorption of Magnesium. Magnesium is absolutely crucial because it helps convert Vitamin D into its active form and is required to regulate the parathyroid hormone, which is involved in maintaining bone mass. A Magnesium deficiency, often caused by excess calcium, directly contributes to poor bone density.
- Calcification of Soft Tissues: This is perhaps the most serious concern. When too much supplemental calcium is consumed—especially without adequate co-factors like Vitamin D3 and K2—the body struggles to incorporate all of it into the bone matrix. This excess calcium can then deposit in soft tissues, including arteries (leading to cardiovascular risk) and cartilage, but also potentially interfere with the bone-building process itself. Geriatricians emphasize that putting calcium into the bones requires an intelligent team of vitamins and supplements, not just a massive dose of one player.
The Cardiovascular Warning: The Silent Threat of Excess Calcium
The risk associated with high-dose supplemental calcium goes beyond just accelerating bone loss—it touches the heart, a major concern for women over 50.
Several large-scale studies have suggested a link between taking high-dose calcium supplements and an increased risk of heart attacks and stroke. The theory is that when calcium is rapidly absorbed from a pill, it can cause transient spikes in blood calcium levels. If not properly channeled to the bones by Vitamin K2, it can end up contributing to the buildup of arterial plaque (arterial calcification), effectively hardening the arteries.
Geriatricians strongly advocate for obtaining calcium from dietary sources first, as the calcium in food is absorbed slowly and naturally alongside other co-factors, minimizing the risk of adverse cardiovascular events. The body processes nutrition from food far more efficiently than it handles a massive chemical bolus from a pill.
The Strategic Solution: Your New Bone Health Team
The solution for women over 50 is not to fear calcium, but to focus on the full bone-building team. Geriatricians suggest a shift in strategy: focus on synergistic co-factors and adequate dietary calcium.
1. Ditch the High-Dose Calcium Pill
Instead of taking 1,000 mg or more of supplemental calcium, aim for the recommended total daily intake (around 1,200 mg for women over 50) primarily through food. Supplements should only be used to fill a verified gap.
2. Prioritize Co-Factor Vitamins
Bone health requires a trio of key vitamins and supplements to ensure calcium is deposited where it belongs:
- Vitamin D3: Absolutely essential for calcium absorption in the gut. Without adequate D3, your high-dose calcium supplement is mostly ineffective. Sun exposure and supplementation are often necessary, especially in northern latitudes.
- Magnesium: As discussed, Magnesium is necessary for D3 activation and bone structure. Good sources include dark leafy greens, nuts, seeds, and quality supplements.
- Vitamin K2 (MK-7): This is the unsung hero. Vitamin K2 activates proteins that specifically direct calcium into the bones and teeth, and away from arteries and soft tissues. Geriatricians view K2 as non-negotiable for safe calcium utilization.
3. Food First: The Best Source of Calcium
Dietary calcium is always the safest and most bioavailable choice. Good sources include:
- Dairy (Yogurt, Cheese, Milk)
- Dark Leafy Greens (Kale, Collard Greens)
- Fortified foods and supplements (like fortified orange juice).
By ensuring a balanced intake of these co-factors, you create an environment where the calcium you consume can actually strengthen your bones, instead of becoming a potential liability.
The Geriatrician’s Simple Bone Health Command
The warning for women over 50 is clear: the intention behind taking high-dose calcium supplements is good, but the execution can be damaging, potentially accelerating bone loss and increasing cardiovascular risk. This is the 1 common supplement to approach with extreme caution.
Your path to longevity and robust bone density relies on a strategic partnership between essential vitamins and supplements. Stop relying solely on massive doses of calcium and start focusing on the powerful team of Vitamin D3, Magnesium, and Vitamin K2 to ensure that every molecule of calcium you consume is directed to its proper place. By listening to the Geriatrician and adopting a balanced approach to your nutrition, you protect your heart and secure the strong, resilient skeletal foundation necessary for a vibrant life after 50.
Related Articles
- New Hope for Alzheimer’s? This Popular Supplement Shows Surprising Promise in Latest Study
- Think Collagen Is Just Hype? These Skin, Hair, and Joint Results Say Otherwise
- I Took Tru Niagen for 30 Days—The Energy, Sleep, and Brain Changes Shocked Me
- The Menopause Sleep Mineral: 90% of Women Are Deficient in the Magnesium That Stops Night Sweats
- 2025 Collagen Guide: What Really Works for Glowing Skin, Strong Joints, and Youthful Aging