FREE SHIPPING OVER $50
Turning 50? Here’s What Happens to Your Teeth—and How to Stop the Damage

You’ve hit a huge milestone! While turning 50 might bring new routines like annual physicals or a greater focus on fitness, many people overlook one critical area that changes profoundly during this decade: their oral health. You may notice that your teeth look different, feel more sensitive, or your gums seem to be receding. These aren’t just cosmetic changes; they’re evidence of biological shifts that require adjusting your daily routine. The habits that kept your teeth healthy in your thirties simply aren’t enough to counteract the effects of fifty-plus years of wear and tear, medications, and natural aging.
The key to maintaining a bright, functional smile well into your later years is understanding these changes and being proactive. We are going to break down the five most common and important ways aging affects your teeth and gums after age 50. More importantly, we’ll give you clear, actionable strategies—backed by dental science—to stop the damage, protect your bone structure, and keep your teeth firmly where they belong. It’s time to upgrade your oral care routine for longevity.
The Core Shift: Why Oral Health Changes After 50
The environment inside your mouth changes significantly around the age of 50 due to a convergence of factors. Primarily, we see structural changes, chemical shifts, and the cumulative effects of decades of use.
1. Gum Recession and Periodontal Disease
This is arguably the most critical and common change affecting oral health in middle age. Gum recession is when the gum tissue surrounding the teeth wears away or pulls back, exposing more of the tooth’s root.
The Damage
- Sensitivity: The exposed tooth root lacks the protective enamel of the crown, making it incredibly sensitive to hot, cold, and sweet foods.
- Root Decay: The root surface is covered in cementum, which is much softer than enamel. This makes the root highly susceptible to cavities, known as root decay. These cavities are often harder to treat and can rapidly compromise the tooth structure.
- Bone Loss: Gum recession is frequently a sign of periodontal disease (gum disease), where chronic inflammation causes the bone supporting the teeth to erode. Bone loss is the number one cause of tooth loss in adults.
How to Stop the Damage
- Master Proper Brushing Technique: Use a soft-bristled toothbrush and brush gently. Scrubbing aggressively accelerates gum recession. Focus on brushing at a 45-degree angle to the gum line, using short, circular strokes. Consider switching to an electric toothbrush with a pressure sensor.
- Prioritize Flossing and Interdental Cleaners: Flossing is your only defense against plaque deep beneath the gum line. Additionally, use interdental brushes or water flossers to clean the exposed root areas and between teeth where recession has created small pockets.
2. Enamel Erosion and Dentin Exposure
Over five decades, the wear and tear from chewing, grinding, and exposure to acidic foods and drinks takes a heavy toll on the hard, protective shell of your teeth: the enamel.
The Damage
- Thinning and Cracking: Enamel thins, making the teeth more prone to chipping, cracking, and fractures—particularly in back teeth where chewing forces are highest.
- Color Change: As the outer white enamel layer wears down, the underlying layer of tissue, called dentin, becomes more visible. Dentin is naturally yellow or brownish. This is the primary reason older adults often notice their teeth darkening.
- Increased Sensitivity: Thinning enamel allows temperature changes and irritants to reach the nerves inside the dentin tubules more easily, increasing overall tooth sensitivity.
How to Stop the Damage
- Fluoride is Not Just for Kids: Use a prescription or high-concentration fluoride toothpaste or rinse. Fluoride actively remineralizes and strengthens the remaining enamel and the vulnerable root surfaces, offering a crucial shield against decay.
- Manage Acid Exposure: Limit highly acidic beverages like soda, citrus juices, and wine. When you do consume them, use a straw and avoid swishing. Wait at least 30 minutes after consuming acid before brushing, as brushing immediately can scrub away acid-softened enamel.
3. Dry Mouth (Xerostomia) and Increased Decay
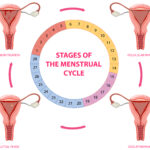
As people reach and pass the age of 50, they often start taking more medications for chronic conditions such as high blood pressure, cholesterol, or depression. Unfortunately, hundreds of common medications list dry mouth (Xerostomia) as a side effect.
The Damage
- Loss of Saliva’s Protection: Saliva is your mouth’s first and best defense. It naturally washes away food particles, neutralizes plaque acids, and contains essential minerals for re-hardening enamel. A dry mouth creates a hostile, highly acidic environment where bacteria thrive, leading to a dramatic increase in the rate of tooth decay and periodontal disease.
- Difficulty Swallowing: Chronic dry mouth makes it harder to chew and swallow, impacting your ability to enjoy food and get proper nutrition.
How to Stop the Damage
- Stay Hydrated: Sip water constantly throughout the day, not just during meals.
- Stimulate Saliva: Chew sugar-free gum or suck on sugar-free candies containing Xylitol. Xylitol not only stimulates saliva but also actively inhibits the growth of cavity-causing bacteria.
- Use Artificial Saliva Products: Your dentist or pharmacist can recommend over-the-counter saliva substitutes or moisturizing mouth sprays designed to coat and soothe tissues and provide immediate relief from dry mouth.
4. Darkening and Embrittlement of Fillings
If you are turning 50, chances are you have amalgam (silver) or composite (white) fillings placed decades ago. These restorations do not last forever, and their deterioration poses a risk to the surrounding tooth structure.
The Damage
- Leaky Margins: Over time, old fillings can shrink, crack, or pull away slightly from the tooth structure, creating tiny gaps called “leaky margins.” These gaps are impossible to clean and become prime targets for bacteria to start new decay beneath the filling.
- Cracked Tooth Syndrome: The continuous stress of chewing on a large, old filling can cause hairline cracks to form in the tooth structure around it. These cracks can lead to intense pain, sensitivity, and, eventually, a fractured tooth, often necessitating a crown or root canal.
- Aesthetic Concerns: Old composite fillings often stain and darken significantly, contrasting sharply with the surrounding teeth.
How to Stop the Damage
- Regular X-rays: Ensure your dentist takes annual or biennial bitewing X-rays. These images are essential for catching recurrent decay under old fillings before it becomes a symptomatic problem that requires major restorative work.
- Replacement: Don’t wait for old, failing fillings to become painful. Proactively discuss replacing large or cracked fillings with newer, stronger materials or crowns to protect the tooth structure for the long term.
5. Increased Risk of Oral Cancer
While this change doesn’t directly affect the structure of your teeth, the risk of oral cancer significantly increases after the age of 45, making it a crucial part of your oral health vigilance after turning 50.
The Damage
- Late Detection: Oral cancer often manifests as seemingly benign red or white patches, non-healing sores, or lumps in the mouth, throat, or on the tongue. When caught late, prognosis drops sharply.
- Impact on Function: Treatment for oral cancer can involve major surgery that permanently affects the ability to speak, chew, and swallow.
How to Stop the Damage
- Bi-Annual Oral Cancer Screenings: Ensure your dental professional performs a visual and tactile oral cancer screening at every single cleaning and checkup appointment. This takes less than two minutes and is life-saving.
- Self-Checks: Become familiar with the tissues in your own mouth. If you notice any sore or lump that hasn’t healed within two weeks, seek an immediate evaluation.
- Limit Risk Factors: Reduce or eliminate tobacco use (smoking or chewing) and limit excessive alcohol consumption, as these are the leading risk factors for oral cancer.
Conclusion
Reaching the age of 50 is a perfect time to pivot your approach to oral health. The five key challenges—gum recession, enamel erosion, dry mouth, failing old restorations, and the increased risk of oral cancer—are formidable, but they are all highly manageable with preventative care. By adopting a gentler but more thorough brushing technique, prioritizing fluoride and Xylitol for daily defense, staying meticulously hydrated, and ensuring you receive regular, comprehensive dental exams, you can actively stop the damage. Your mouth is a critical indicator of your overall health and well-being; investing in its care after turning 50 is one of the best choices you can make for a healthy, comfortable, and independent longevity.
Related Articles
- Scientists Use Sheep’s Wool to Repair Teeth—This Natural Protein Could Replace Fillings
- 7 Everyday Habits That Quietly Destroy Your Teeth—Dentists Say #4 Is the Worst
- Before You Book That Root Canal—Here’s What You Need to Know About Safer, Easier Options
- Brushing Before or After Breakfast? Dentists Say Most People Get This Wrong
- Hate Flossing? Dentists Recommend This Surprisingly Easy Alternative