FREE SHIPPING OVER $50
Lying Down for a Blood Pressure Check Reveals Hidden Heart Risk — What Doctors Miss

Most of us know the drill: you walk into the doctor’s office, sit on the edge of the exam table with your feet dangling, and wait for the cuff to squeeze your arm. If the numbers come back at 120/80, you get a pat on the back and a “see you next year.” We’ve been conditioned to believe that this single, seated snapshot is the definitive word on our cardiovascular health. However, recent medical research suggests that this traditional method might be giving millions of people a false sense of security. It turns out that your posture during a blood pressure check can hide—or reveal—dangerous heart risks that are completely invisible while you are sitting up.
The Science of Gravity and Your Heart
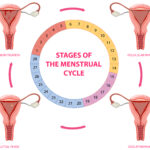
To understand why lying down changes the game, we have to look at how gravity affects your blood flow. When you are standing or sitting, gravity pulls your blood toward your lower extremities. Your heart has to work against that pull to get oxygen-rich blood to your brain. To compensate, your blood vessels constrict slightly to maintain pressure.
However, the moment you lie down, gravity is no longer a factor. The blood that was pooling in your legs rushes back toward your heart and torso. In a perfectly healthy system, your baroreceptors (pressure sensors in your neck and chest) signal your heart to slow down and your vessels to relax. But if those sensors are “stiff” or if your arteries have lost their elasticity, the pressure spikes instead. This is why a person can have a perfect reading while sitting, yet be in a “danger zone” the moment they go to bed.
Why the “Sitting Test” Fails So Many People
The medical community has relied on seated tests for decades, primarily for convenience. It’s easier to take a reading while a patient is already sitting in a chair. But a study presented at the American Heart Association’s Scientific Sessions revealed that a significant percentage of people with “normal” seated blood pressure actually had hypertension when measured lying down.
These individuals, often referred to as “masked hypertensive” patients, have the same long-term risks for heart failure and stroke as those with obvious high blood pressure. Because their risk is “masked” by their posture during office visits, they often go years without treatment.
| Measurement Posture | What It Detects | What It Might Miss |
| Seated (Standard) | Daytime baseline pressure | Nighttime spikes (Supine Hypertension) |
| Standing | Orthostatic Hypotension (Dizziness) | True resting arterial tension |
| Lying Down (Supine) | Hidden vascular resistance | Nothing—this is the most “raw” reading |
The Link Between Lying Down and Nighttime Strokes
Why does supine hypertension matter so much? Most cardiovascular events, including strokes and heart attacks, occur in the early morning hours or during sleep. If your blood pressure spikes when you lie down, your heart is struggling for the 7 to 9 hours you are in bed.
High pressure during sleep is particularly damaging because it prevents the “nocturnal dip.” Normally, your blood pressure should drop by about 10% to 20% while you sleep. This dip gives your arteries a much-needed break. If you have hidden heart risks revealed by a lying-down test, your arteries never get that rest. Over time, this constant pressure leads to:
- Left Ventricular Hypertrophy: The heart muscle thickens and becomes less efficient.
- Arterial Scarring: High pressure causes micro-tears in the artery walls where plaque can build up.
- Kidney Strain: The kidneys are highly sensitive to pressure changes and can begin to fail if nighttime pressure remains high.
Who Is Most at Risk for Hidden Heart Risks?
Not everyone needs to panic, but certain groups are much more likely to show these “hidden” numbers when they lie down. As we age, our “autonomic nervous system”—the part of the brain that controls automatic functions like blood pressure—starts to lose its precision.
Specifically, people with Type 2 diabetes often have damaged nerves that can no longer signal the blood vessels to relax when gravity changes. Similarly, those with obstructive sleep apnea or chronic kidney disease should be especially vigilant. If you find yourself waking up with a dull headache or feeling “puffy” in the morning, these could be signs that your nighttime blood pressure is higher than your daytime seated reading suggests.
How to Perform the “Posture Check” at Home
You don’t have to wait for your next annual physical to find out if you’re at risk. If you have a home blood pressure monitor, you can conduct your own 2-step assessment. This is a powerful way to advocate for your health when you next speak with your doctor.
- The Seated Baseline: Sit quietly for 5 minutes with your feet flat on the floor and back supported. Take three readings and average them.
- The Supine Test: Lie flat on your back on a bed or sofa for at least 5 to 10 minutes. Ensure your arm is supported at the same level as your heart (use a small pillow if needed). Take three readings and compare them to your seated average.
The Red Flag: If your systolic number (the top one) is significantly higher (10 points or more) while lying down compared to sitting up, you may have supine hypertension. This is a crucial data point to share with a cardiologist.
Why Doctors Often “Miss” This Vital Metric
It isn’t that doctors are being negligent; it’s that the system is built for speed. A typical primary care appointment lasts 15 minutes. Spending 10 of those minutes waiting for a patient to reach a “resting state” while lying down simply doesn’t fit the standard workflow.
Furthermore, many automated machines in clinics are calibrated for a seated position. Transitioning to a lying-down protocol requires extra space and time that most clinics aren’t currently equipped for. This is why being a “proactive patient” is so important. By bringing your own home data to the table, you force the conversation toward a more comprehensive view of your heart health.
Correcting the Risk: Life After a High Supine Reading
If you discover that your blood pressure spikes when you lie down, the good news is that it is manageable. Doctors often treat supine hypertension by adjusting the timing of medication. For instance, taking blood pressure medication at night rather than in the morning can ensure the drug is at its peak effectiveness while you are horizontal.
Lifestyle shifts can also make a massive difference. Sleeping with a slight incline (using a wedge pillow) can prevent the sudden rush of blood to the heart that triggers the pressure spike. Reducing sodium intake in the evening and ensuring you are well-hydrated throughout the day also helps the baroreceptors function more smoothly.
Related Articles
- Stop Saying “I’m Too Old” — 6 Toxic Thoughts That Speed Up Aging
- The “Can Your Toes Do This? It Might Predict How Long You’ll Live”
- The “Laughter Shield”: The Surprising Way Joy Floods Your Brain with Alzheimer’s-Fighting Chemicals
- The Bone-Density Myth: Why 70% of Adults Are Silently Starving Their Skeleton (The New Protein Rule)
- Researchers Reveal: The Overlooked Supplement That Could Shield Your Brain From Dementia