FREE SHIPPING OVER $50
Is Alzheimer’s Actually Type 3 Diabetes? What Doctors and Researchers Are Now Saying

For a long time, we thought of Alzheimer’s disease as an unavoidable genetic curse—a cruel fate determined by our DNA. The very idea of it can be terrifying, a creeping shadow that threatens our memories, our personalities, and our very essence. However, what if that view is completely wrong? A growing number of doctors and researchers are now challenging this conventional wisdom, proposing a radical new theory: that Alzheimer’s is a metabolic disease, a form of diabetes that affects the brain. This is not just a clever metaphor; it is a profound scientific re-evaluation that could change the way we think about longevity and cognitive health.
This theory, which has led to the informal term “Type 3 Diabetes,” suggests that the same processes that cause high blood sugar and insulin resistance in the body also drive the devastating decline of the brain. While it is not yet an official diagnosis, the research is so compelling that it is reshaping the entire conversation around dementia. In this article, we’ll explore the evidence behind this theory, reveal the critical connection between insulin and your brain, and provide actionable steps you can take to protect your mind for years to come.
The Brain on Sugar: Why Alzheimer’s is Being Called ‘Type 3 Diabetes’
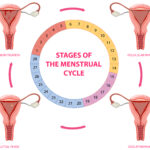
The term “Type 3 Diabetes” was first proposed to describe Alzheimer’s disease because the brains of people with Alzheimer’s show a profound deficiency in insulin and a resistance to it. Just as Type 2 Diabetes results from insulin resistance in the body, leading to high blood sugar, Alzheimer’s appears to stem from insulin resistance that occurs specifically in the brain. This metabolic breakdown starves brain cells of their primary fuel source: glucose.
In a healthy brain, insulin plays a vital role far beyond just managing glucose. It helps nerve cells communicate with each other, promotes their growth, and helps them survive. But when brain cells stop responding to insulin, they can no longer get the energy they need to function. The result is a progressive decline in cognitive abilities, mirroring the classic symptoms of Alzheimer’s, such as memory loss, confusion, and difficulty with daily tasks.
This is not a peripheral issue; it is a central part of the disease. In fact, studies using brain scans have shown that a decline in glucose metabolism in the brain can be detected years, and even decades, before any cognitive symptoms of Alzheimer’s appear. This means that the metabolic dysfunction is not a symptom of the disease but a potential cause, positioning it as an early warning sign that we can now recognize and, hopefully, address.
The Insulin-Alzheimer’s Connection: A Vicious Cycle
The link between insulin resistance and Alzheimer’s is not a coincidence; it is a complex, biological partnership that creates a devastating feedback loop.
Insulin’s Role in Clearing Brain Toxins
Your brain has a built-in waste removal system. One of the key players in this system is an enzyme called insulin-degrading enzyme (IDE). This enzyme is responsible for breaking down and clearing out two things: excess insulin and the notorious amyloid-beta plaques that are a hallmark of Alzheimer’s disease.
The problem is that IDE is not designed to handle both jobs at once. When you have chronic high insulin levels—a common result of a diet rich in sugar and refined carbohydrates—the IDE enzyme becomes overwhelmed. It prioritizes clearing the excess insulin, which is a more immediate threat to your body, and as a result, it neglects its other job of clearing the amyloid-beta plaques. Over time, these plaques build up and clump together, blocking nerve cell communication and leading to widespread brain cell death.
The Brain’s Energy Crisis
In a similar vein, the brain’s ability to use glucose is directly linked to insulin sensitivity. When your brain becomes resistant to insulin, glucose uptake is significantly reduced. This puts your brain cells in a state of crisis. They are essentially starving for energy, which hinders their ability to perform basic functions like forming and retrieving memories. This energy crisis also increases oxidative stress, which further damages brain cells and accelerates neurodegeneration.
Furthermore, the same insulin resistance that starves the brain can also trigger inflammation, a well-known contributor to dementia and other neurodegenerative diseases. Chronic inflammation creates a hostile environment for brain cells, making them more vulnerable to damage and death.
The Lifestyle Link: How Diet and Habits Impact Your Brain’s Health
If Alzheimer’s is, in part, a metabolic disease, then the good news is that we can influence our metabolic health through our lifestyle choices.19 The same habits that lead to Type 2 Diabetes are the ones that can set the stage for cognitive decline.
The Problem with the Modern Diet
Our modern diet, often high in processed foods, refined carbohydrates, and sugar, drives chronic insulin spikes. When you eat a bowl of sugary cereal for breakfast, your blood sugar and insulin levels surge. Over time, this constant demand on your body and brain leads to insulin resistance, setting you on a path toward metabolic dysfunction. This is not a message of blame; it is one of empowerment. It means that the path to a healthier brain begins with what you put on your plate.
The Power of Exercise
Physical activity is one of the most powerful tools we have to improve insulin sensitivity, not just in our muscles but in our brains. Regular exercise, especially a mix of cardiovascular activity and strength training, helps your cells become more responsive to insulin, allowing them to use glucose more efficiently. It also promotes blood flow to the brain, which delivers oxygen and nutrients essential for cognitive function.
The Importance of Sleep
Poor sleep is another major contributor to insulin resistance. Studies have shown that even one night of poor sleep can significantly decrease your body’s ability to handle glucose. This is especially true for deep sleep, which is when your brain performs a kind of “detoxification” process, clearing out waste products and cellular debris. Without adequate, restorative sleep, your brain’s ability to clean itself becomes compromised, which can contribute to the buildup of the very plaques associated with Alzheimer’s.
A Path to Brain Longevity: Taking Control
The “Type 3 Diabetes” theory gives us a new and hopeful perspective on longevity and brain health. It shows us that we are not helpless in the face of dementia. By focusing on our metabolic health, we can actively work to protect our minds.
Adopt a Brain-Healthy Diet
Make a conscious choice to eat foods that keep your blood sugar and insulin levels stable.
- Cut Down on Sugar and Refined Carbs: Replace sugary drinks, white bread, and pastries with whole foods like vegetables, fruits, and legumes.
- Embrace Healthy Fats: Include sources of healthy fats like avocados, nuts, seeds, and olive oil in your diet. The brain is composed of a significant amount of fat, so providing it with the right kind of fuel is crucial.
- Prioritize Protein: Eat lean proteins and fatty fish, which are not only good for muscle maintenance but also help with satiety and blood sugar regulation.
Stay Active, Mentally and Physically
- Get Moving: Aim for at least 30 minutes of moderate-intensity exercise most days of the week. This can be as simple as a brisk walk.
- Challenge Your Mind: Keep your brain engaged by learning new skills, solving puzzles, and staying socially connected. These activities promote the growth of new neural connections and help your brain stay resilient.
Conclusion
The idea of Alzheimer’s as “Type 3 Diabetes” is a powerful one because it shifts our focus from an incurable condition to a potentially preventable one. It is not an official medical diagnosis, but a scientific framework that is fundamentally changing how doctors and researchers view the disease. It tells us that the state of our metabolic health is directly linked to the health of our brain, and that the choices we make every day—what we eat, how much we move, and how we sleep—have a profound impact on our cognitive longevity. By understanding and acting on the insulin-brain connection, you can empower yourself to protect your mind and pursue a life of cognitive vibrancy.
Related Articles
- Doctors Are Stunned: These 15 Mobility Tricks Have Seniors Moving Like They’re 30 Again
- 10 Exercises That Could Be Dangerous After 60—Most People Still Do #7
- Can’t Sit Cross-Legged? Try These Trainer-Approved Standing Hip Stretches
- Transform Your Body After 50: Top Exercise Habits Revealed
- Defy Age: 13 Surprising Tips Making 60-Year-Olds Stronger Than Millennials